You notice shortness of breath and a stark pain in your chest. You might have lost your taste and smell and you are breathing like you just walked up three flights of stairs. You can’t talk in full sentences. These symptoms signal a trip to the emergency department of your local hospital.
Before you rush in, call your doctor or hospital ahead and describe your symptoms. This is because your local emergency clinic might not have enough beds and may need to direct you to another facility. Or your symptoms might not be considered severe enough yet to require treatment at the hospital. So it’s best to check in by phone first.
But once admitted, nurses will give you a COVID-19 test by putting a 15 centimeter (6 inch) cotton swab up both sides of your nose or your throat for about 15 seconds. Most patients will also have a set of blood tests taken from their veins. Doctors will then listen to your lungs and check the levels of oxygen in your blood with a clip-on finger monitor.
Why are they doing that? Because if you have severe COVID-19 symptoms the oxygen levels in your blood can drop too low. Since this can result in life-threatening damage to your vital organs, you’ll get oxygen to breathe through two small tubes that go just inside your nostrils or through a facemask.
You will then get a chest X-ray or a CT scan so that doctors get a better understanding of which areas of your lungs are inflamed.
A CT scan, also known as computerized axial tomography, is a painless diagnostic test that uses X-rays and computers to create cross-sectional images of your body. A CT scanner is a large square or round X-ray machine with a tunnel through the center, it helps doctors see into your lungs. During your CT scan, you will lie on a table that slowly passes through the tunnel. A giant ring called a gantry will rotate around your body. It contains a tube that releases X-ray beams and detectors that will measure the amount of radiation absorbed by your body, and these beams will capture many views of your body from different angles. As the gantry spins the detectors will send data to a computer that creates cross-sectional images or 3D models of your lungs, helping doctors diagnose the severity of your coronavirus infection. Now your doctors have all the data to determine the progress of your COVID-19 infection.
What treatments can improve your condition?
Some patients may get standard antibiotics. These won’t fight the coronavirus directly but could be beneficial if you develop an additional bacterial infection in your lungs. But because there is no approved medicine specifically for COVID-19 you’ll be relying on your immune system to fight off the virus and hope that oxygen therapy combined with supportive care can help your body recover.
If things go your way, your immune system will start to produce antibodies to slowly kill the virus. But what happens if your condition worsens?
In that case, you will probably experience severe breathing problems, high fever, profound headaches, and nausea. If the oxygen concentration in your blood then drops below critical levels, doctors can escalate your treatment to something called high-flow nasal oxygen, which means that a machine will be pushing air into your nose, warmed to body temperature and humidified with sterile fluid. You can so get up to 60 liters of oxygen per minute and up to 100% concentration compared to 15 liters oxygen per minute to a concentration of only 60% with standard oxygen therapy through medical face masks.
There are concerns however that this can put viruses into the air and potentially infect other patients, caregivers or anyone nearby. To counter this risk, some hospitals have negative pressure rooms. These are isolation rooms equipped with a special ventilation system that generates negative pressure by allowing air to flow in but not to leave the room. The air is then ventilated to the outdoors through a filter system. The bad news is that not every hospital has these rooms, so high flow nasal oxygen might not be an option.
So what other options do your doctors have?
If high-flow nasal oxygen is not an option or didn’t help, doctors will start you on mechanical ventilation in a last life-saving effort.
Before you are intubated and ventilated, you will be given medication via IV to put you to sleep. The first step in mechanical ventilation is called endotracheal intubation. Once you are asleep your doctor will use an instrument called a laryngoscope. This device helps guide the endotracheal tube to its proper position. Your doctor will tilt your head back slightly and insert the laryngoscope through your mouth and down into your throat, taking special care to avoid contact with your teeth using a special blade on the device. Your doctor will gently raise the epiglottis, which is a flap of tissue protecting your larynx, as they advance the tip of the endotracheal tube into the trachea. Once the tube is in place, your doctor will inflate a small balloon surrounding the tube to make sure it remains snugly in place. They will then remove the laryngoscope and tape the tube to the corner of your mouth to prevent it from being jostled out of position.
Your doctor will check to see that the tube is properly positioned in the lower part of the windpipe by inflating your lungs with a special bag and listening for breathing sounds on both sides of your chest. If the end of the tube is too low, both lungs will not receive the same amount of air. In some cases, an X-ray is taken immediately after intubation to confirm the placement of the tube. Once the endotracheal tube is in the proper position, your doctor will attach it to the mechanical ventilator, which will have a specially designed pump that aids respiration by delivering well-oxygenated air into the lungs and permitting carbon dioxide to escape. Levels of oxygen and carbon dioxide will be closely monitored to confirm that the ventilator is working properly.
Now, you’re asleep and a machine is managing your breathing.
What are your chances of survival at this stage?
Unfortunately, according to infectious disease expert Dr. Dennis Carroll, former head of the U.S. Agency for International Development’s Emerging Pandemic Threats program, only around one-third of those COVID-19 patients placed on ventilators survive. Ventilators can also be damaging to a patient when used over long periods of time. So if you do make it through this, you will have a long road of recovery in front of you.
At the beginning of the outbreak, some hospitals were putting patients on ventilators early on in their treatment. This was due in part to concerns over less invasive procedures could cause viral particles into the air. With more cases of COVID-19 to study, health professionals are attempting to set guidelines for different types of respiratory failure and who ventilator treatment would be best suited for. This includes recommendations such as placing patients on their stomachs — called prone positioning – which evidence suggests helps increase the amount of oxygen that’s getting to their lungs.
Why does this virus cause only mild disease in most people, but could turn fatal for you despite being healthy?
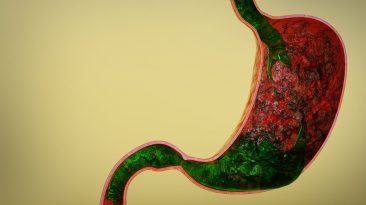
In such a case, it seems the worst damage may be caused by an abnormal immune response to the infection rather than the virus itself. In simplified terms, when any cell in your body senses that there is something foreign, in this case, a virus, the immediate response of the cell is to kill itself, a protective mechanism to prevent it from spreading to other cells.
The way this happens is that cells in your immune system called macrophages release small signaling proteins called cytokines. Certain kinds of these trigger cell death. When many cells are doing this at the same time a lot of tissue can die. This is what medical professionals call a cytokine storm.
In COVID-19 this means that lung tissue breaks down and the walls of the lungs’ tiny air sacs leak fluid through, so causing pneumonia and starving the blood of oxygen. Basically, most of your cells in the tissue will die as a result of this uncontrolled level of cytokines. It eats away at your lungs to a point where they cannot recover. Your body is now attacking itself.
Cytokine storms are becoming a common occurrence in COVID-19 patients with severe symptoms and they seem to play a role in death in a large number of cases.
Whether you would develop a cytokine storm may depend on genetic factors. Patients in studies with the H1N1 influenza virus who developed cytokine storm syndrome, often possessed subtle genetic immune defects resulting in the uncontrolled immune response. Now, you are more likely to have developed these genetic immune defects as you age but there is also a small chance that you might have a genetic predisposition to developing cytokine storms after infection with the novel coronavirus.
It’s important to mention that the complete picture of cytokine storms is not yet well understood and the medical community is still early in understanding the many aspects of the disease. A lot of findings and hypotheses need to be confirmed in more and larger clinical studies.
But the good news is that many clinical trials are underway to explore treatments used for other conditions that could halt cytokine storms and fight COVID-19 as well as to develop new ones. Several studies are focused on an antiviral medication called remdesivir, which was created to fight Ebola. There are currently hundreds of clinical trials of proposed COVID-19 drugs already recruiting patients.
So, if you’re lucky enough and make it through all this you’ll be weaned off the ventilator. You will probably feel extremely exhausted but you can now step down to a normal hospital ward from critical care, where you stay until you can maintain safe oxygen levels by just breathing air before discharged home and reunited with your loved ones.
Special thanks to Nucleus Medical Media for providing the 3D animations in the video above.
References:
- 2020. WHO.int Accessed April 17 2020.
- Canada, Public. 2020. “Clinical Management Of Patients With Moderate To Severe COVID-19 – Interim Guidance – Canada.ca“. Canada.ca. Accessed April 17 2020.
- “COVID-19 Transmission Assessment Report | Vapotherm – Mask-Free NIV For Spontaneously Breathing Patients”. 2020. Vapotherm – Mask-Free NIV For Spontaneously Breathing Patients. Accessed April 21 2020. .
- “How Does The Coronavirus Kill?“. 2020. Nature.Com. Accessed April 15 2020.
- “The Coronavirus Patients Betrayed By Their Own Immune Systems“. 2020. Nytimes.com. Accessed April 15 2020.
- Tisoncik, J. R., M. J. Korth, C. P. Simmons, J. Farrar, T. R. Martin, and M. G. Katze. 2012. “Into The Eye Of The Cytokine Storm“. Microbiology And Molecular Biology Reviews 76 (1): 16-32. American Society for Microbiology. doi:10.1128/mmbr.05015-11.
- Windsor, Matt. 2020. “Here’s A Playbook For Stopping Deadly Cytokine Storm Syndrome – The Reporter”. Uab.Edu. Accessed April 15 2020.
- Schulert, Grant S., Mingce Zhang, Ndate Fall, Ammar Husami, Diane Kissell, Andrew Hanosh, and Kejian Zhang et al. 2015. “Whole-Exome Sequencing Reveals Mutations In Genes Linked To Hemophagocytic Lymphohistiocytosis And Macrophage Activation Syndrome In Fatal Cases Of H1N1 Influenza“. Journal Of Infectious Diseases 213 (7): 1180-1188. Oxford University Press (OUP). doi:10.1093/infdis/jiv550.
- “Which Covid-19 Drugs Work Best?“. 2020. MIT Technology Review. Accessed April 17 2020.
- Discovery, Nature. 2020. “John-Arne Røttingen“. Nature.Com. Accessed April 17 2020.
- Wang, Manli, Ruiyuan Cao, Leike Zhang, Xinglou Yang, Jia Liu, Mingyue Xu, Zhengli Shi, Zhihong Hu, Wu Zhong, and Gengfu Xiao. 2020. “Remdesivir And Chloroquine Effectively Inhibit The Recently Emerged Novel Coronavirus (2019-Ncov) In Vitro“. Cell Research 30 (3): 269-271. Springer Science and Business Media LLC. doi:10.1038/s41422-020-0282-0.
- “For Survivors Of Severe COVID-19, Beating The Virus Is Just The Beginning“. 2020. Science | AAAS. Accessed April 17 2020.